New research to be presented at this year’s European Congress of Clinical Microbiology and Infectious Diseases (ECCMID 2024) in Barcelona, Spain (27-30 April) details the case of a man who had received two doses of the monkey pox vaccine in Autumn, 2022 yet experienced a ‘breakthrough’ mpox infection in January 2024.
The authors believe breakthrough should be considered in fully vaccinated individuals engaging in high-risk behaviors. They also call for further research on the need for booster doses to protect against these breakthrough infections.
The case report is by Dr Luigi Segagni-Lusignani, Public Health Authority, Vienna, Austria and colleagues. They add a second case, reported in the last few weeks (March 2024) is currently under investigation.
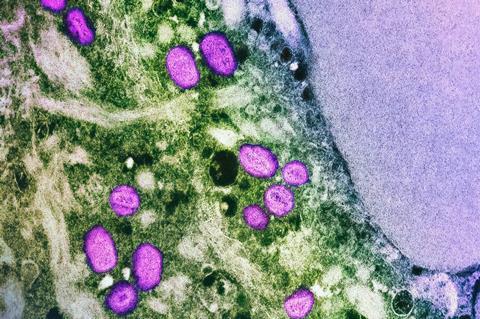
Upsurge in mpox
Following the sharp decline in notifications of new mpox infections after introducing the EMA-approved modified Vaccinia Ankara–Bavarian Nordic (MVA-BN) administration in late 2022 and early 2023, an upsurge in mpox cases occurred in the latter half of 2023 in European countries. Clusters were observed in individuals presumed immune through recent vaccination, but data on the durability of protective immunity after complete 2-dose vaccination are limited.
The authors here present a case of mpox infection in a 35-year-old, who had completed the two-dose course of intradermal third-generation Jynneos vaccine as pre-Exposure Prophylaxis (PrEP) on November 8, 2022, with a 28-day interval between the first and second dose.
His medical history included well-controlled HIV infection since 2011 (CD4 count of > 700 cells/µL), hepatitis C infection in April 2017, SARS-CoV-2 infection in November 2020, and Campylobacter infections in August 2021 and January 2022.
New case
In January 2024, five days after multiple sexual encounters during a Vienna event, the patient reported fever, chills, headache, discomfort urinating, diarrhoea with bleeding, and penile and anal itching. On day 3, a genital herpes infection was suspected, but no treatment was started. After two days, he presented to the dermatology clinic with worsening lymphadenopathy (swollen lymph nodes), where positive mpox virus PCR results were obtained. His Mpox Severity Score System (MPOX-SSS) was 10 (of a maximum score of 12).
No antiviral treatment was administered, no hospitalisation was required and the patient was home isolated. After 21 days, a control swab was still positive and the isolation had to be extended to day 25 from symptom onset, when finally all scabs fell off the lesions and PCR test on viral swab was negative.
First breakthrough case
The authors say: “This was Austria’s first mpox breakthrough case. Despite no hospitalisation, the clinical course was not less severe than in unvaccinated patients, with longer disease duration and higher scores on the mpox severity scale. The 14-month interval between complete vaccination and infection suggests vaccine-induced immunity could be not durably protective.
This case underscores the importance of clinical suspicion for mpox in high-risk groups, even if fully vaccinated with 2-doses. Breakthrough infections need to be explored further, as well as the possibility of vaccine boosters in vaccinated groups with epidemiological risky behaviours.”
They add: “The Austrian Vaccine Board updates its national mpox vaccine strategy annually based on new scientific evidence. Currently, there is no nationwide recommendation for booster shots after completing the currently recommend (Jynneos) vaccination regimen, even for high-risk groups. However, any potential changes to the vaccination strategy will depend on filling critical knowledge gaps in mpox immunity. These gaps include understanding the current level of immunity, the durability of immune responses, and the long-term vaccine effectiveness in high-risk groups.”







No comments yet