Delivering the two-dose mpox vaccine, called JYNNEOS, in smaller than the usual FDA-approved doses, and by injection between layers of the skin rather than by the standard route under the skin, produced a detectable immune response, a new study shows. This also occurred regardless of whether people were living with or without HIV.
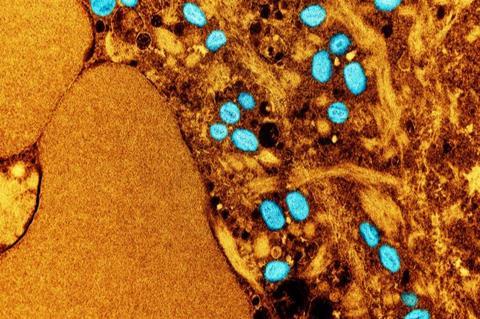
Led by researchers at NYU Grossman School of Medicine, the study showed no significant difference in the strength of the immune response (as gauged by the amount of detectable IgG antibodies, immune proteins that help kill the mpox virus) between most of those who received their vaccine injections in small doses between layers of the skin (intradermally) and those who received it as prescribed in full-dose injections just beneath the skin (subcutaneously). Because of limited space between skin layers, intradermal injections can only accommodate small doses, while larger doses generally require subcutaneous injections.
The smaller doses, about one-fifth of the usual full dose and spread out by as long as three months, were designed to stretch the short supply of vaccine available after an outbreak in May 2022. The IgG antibodies were detected in some cases more than six months after a second and final dose of the vaccine.
Vaccine shortage
The smaller-dose regimen of the JYNNEOS vaccine, which was originally designed to protect against smallpox, an mpox relative, but known to be effective against mpox, was approved during the shortage by the United States government in August 2022. Mpox infection in a small number of cases can be life-threatening.
More than 3,800 New York City residents were infected with the virus, spread by bodily fluids and skin contact, including during sex, and mostly over the course of the outbreak in the summer of 2022. The mpox vaccine is now routinely recommended by the Centers for Disease Control and Prevention (CDC) for people at risk. About 155,000 New Yorkers were vaccinated during this time, mostly using smaller doses.
Threat of outbreak
Researchers say that a resurgence in the Democratic Republic of the Congo in November, with nearly 13,000 suspected cases and some 600 deaths, poses the risk of another outbreak beyond Africa, to other regions and to New York City in particular.
Reporting in the New England Journal of Medicine online Dec. 14, researchers say they found that people fully vaccinated with two smaller doses had an immune response four times stronger than those who did not complete the vaccination series and had only one dose.
“Our study shows that smaller vaccine doses of mpox vaccine administered in two doses, spread out over weeks to months, were similar to the full (subcutaneous) FDA-approved dose,” said study co-lead investigator and infectious disease specialist Angelica Cifuentes Kottkamp, MD. “Implementing the smaller dose was a good emergency measure in the face of immediate shortages of the vaccine,” said Kottkamp, who is an assistant professor in the Department of Medicine at NYU Langone Health.
Smallpox vaccination
Among its other findings, the study showed that those previously vaccinated against smallpox, as part of routine childhood vaccination programs, also had a stronger immune response than those who had had no previous smallpox vaccination. Levels of detectable IgG antibodies in blood samples were 2.7 times higher among those previously vaccinated against smallpox (and then additionally received the JYNNEOS vaccine) compared to those who were not dually vaccinated.
Because of their weakened immune systems, people living with HIV are particularly vulnerable to co-infection. The study found no difference in the magnitude of the immune response between vaccinated people living with HIV (with immune CD4 cell counts above 200) and vaccinated people who are HIV negative.
Valuable support
“Our findings offer valuable support to the people most at risk of being infected with mpox that in the case of an mpox resurgence, infectious disease specialists have sufficient vaccination tools and knowledge to deal with it effectively in the short term,” said study senior investigator Mark Mulligan, MD.
Mulligan, the Thomas S. Murphy Professor in the Department of Medicine at NYU Langone Health, where he also serves as the director of its vaccine center and Division of Infectious Diseases, says more research is needed to determine if additional vaccine doses against mpox are needed for “optimal” protection and to know how long, in months or years, protection lasts. The amount of emergency stockpiles of mpox vaccine and/or the ability to ramp up vaccine production quickly in case of future outbreaks, he notes, also need to be examined.
Some 145 New Yorkers vaccinated against mpox participated in the new study. Most were men (81%), and almost all (89%) self-identified as being LGBTQ+. Thirty-five (24%) were people living with HIV, and 29 (20%) had previously been vaccinated against smallpox.
Public health emergency
The global public health emergency declared by the World Health Organization as a result of the mpox viral outbreak ended in May 2023, one year after it started. However, infections continue to occur globally, with more than 91,000 confirmed cases as of Oct. 31 this year, including 167 deaths in 116 countries. In the U.S., more than 31,000 have been infected, according to the CDC, with 55 deaths. More than 1.2 million doses of the mpox vaccine have been administered in the U.S.
Funding support for the study was provided through National Institute of Health grants R01AI148574 and 75N93021C00014, the New York City Department of Health and Mental Hygiene, and the Blavatnik Family Foundation.
Besides Kottkamp and Mulligan, other NYU Langone researchers involved in this study are co-lead investigators Marie Samanovic-Gordon, PhD, and Ralf Duerr, MD, PhD; and study co-investigators Aaron Oom, PhD, and Hayley Bell, PhD. Other study investigators are Jane Zucker, MD, MSc, and Jennifer Rosen, MD, at the NYC Department of Health and Mental Hygiene.





No comments yet