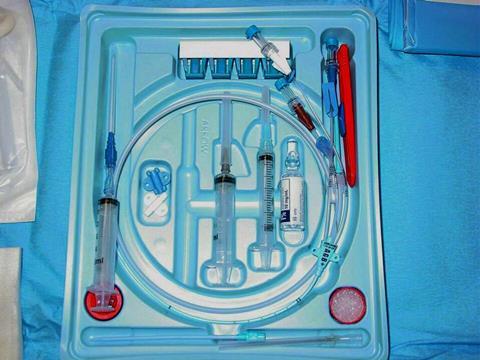
Critically ill patients in intensive care units (ICUs) often depend on central venous catheters, which not only deliver life-saving medications directly into the bloodstream but also are vital tools for assessing cardiovascular function and purifying blood.
While these catheters are indispensable in critical care, their widespread use often poses risks of serious bloodstream infections such as the central line-associated bloodstream infection (CLABSI), a complication that leads to increased mortality rates, longer hospitalization, and higher healthcare costs. This heightened risk of infection highlights the need for standardized, evidence-based safety practices in catheter use.
To address this issue, a team of clinicians, including Dr. Yan Kang from West China Hospital of Sichuan University, Dr. Xiangdong Guan from the First Affiliated Hospital, Sun Yat-sen University, and Dechang Chen from Shanghai Jiaotong University, School of Medicine, along with a working group from the CSCCM, proposed updated guidelines to standardize the clinical practices addressing CLABSI. The guidelines were made available online in the Journal of Intensive Medicine in parts 1 and 2 on January 22, 2026.
“Central line-associated bloodstream infections remain a major challenge in ICUs. We aimed to standardize the clinical practices to reduce infection rates and improve the outcomes for critically ill patients,” says Dr. Chen.
Revised guidelines
The revised guidelines expand on the previous recommendations, which were first issued in 2007, reflecting decades of research. The update was led by a multidisciplinary panel of experts experienced in critical care, evidence-based medicine, biostatistics, and medical informatics. Once the key clinical questions were identified, the team conducted extensive literature review and meta-analyses. They then evaluated the strength of the available evidence and finalized the recommendations with expert consensus and structured voting.
The guidelines present about 52 recommendations for adult ICU patients that are on central line catheters. The recommendations are divided into two complementary parts; one addresses the diagnosis and prevention, while the other focuses on catheter management following infection and appropriate antimicrobial use. Overall, it provides clinicians with a structured framework to reduce infection risk and guide treatment decisions.
“Proper diagnosis is critical for effective CLABSI management,” emphasizes Dr. Chen. “Whenever infection is suspected, we recommend collecting blood specimens from both peripheral veins and catheter hubs to improve diagnostic reliability.”
Focus on prevention
The recommendations majorly focus on prevention. Research shows that the site of catheter insertion significantly influences the risk of infection. For instance, insertions in subclavian veins (located beneath the collarbone) are generally associated with lower risks of infection compared to femoral veins (in the upper thigh) or internal jugular veins (in the neck). Additionally, routine ultrasound guidance during catheter placement is also strongly recommended, as it improves accuracy, increases first-attempt success, and reduces infection-related complications.
“Many catheter-related infections are preventable if the recommended strategies are implemented properly. Our guidelines cover everything from early risk recognition to catheter selection to adherence to aseptic techniques,” note the authors.
READ MORE: A mint idea becomes a game changer for medical devices
READ MORE: The (not so) wonderful world of catheter-associated urinary tract infections
The guidelines identify device selection and maintenance as critical components for infection control. According to the guidelines, clinicians are encouraged to use catheters with the fewest lumens necessary, as additional channels create more opportunities for microbial contamination. Additionally, antimicrobial-coated catheters and chlorhexidine-based skin preparations could also prove effective to limit bacterial growth. Sterile transparent dressings protect the insertion site and allow easy monitoring, while timely changes help prevent infection and skin damage.
Daily clinical reassessment
Further, the guidelines emphasize the importance of daily clinical reassessment, advising prompt removal of catheters that are no longer required to minimize infection risk. Routine blood sampling through the central lines is also discouraged unless clearly indicated. For high-risk patients, additional measures such as antimicrobial lock solutions and daily chlorhexidine bathing are also recommended to suppress the bacterial growth.
Overall, the updated guidelines turn robust research into practical recommendations to standardize catheter use, improve infection prevention, and enhance outcomes for critically ill patients. Dr. Chen concludes, “As critical care continues to evolve, we hope these guidelines will support clinicians in delivering safer and more effective care.”
Topics
- Asia & Oceania
- catheter-related infections
- central line-associated bloodstream infections
- Clinical & Diagnostics
- critical care
- Dechang Chen
- First Affiliated Hospital, Sun Yat-sen University
- Infection Prevention & Control
- Infectious Disease
- intensive care units
- Medical Microbiology
- One Health
- Research News
- Shanghai Jiaotong University, School of Medicine
- West China Hospital of Sichuan University
- Xiangdong Guan
- Yan Kang






No comments yet