Researchers from the German Cancer Research Center (DKFZ) have collaborated with the SILVACX project group at Heidelberg University to develop a therapeutic vaccination concept that can mobilize the immune system to target cancer cells. The team showed that virus peptides coupled to silica nanoparticles can elicit effective T-cell responses against HPV-related tumors. In a mouse model, the nanoparticle-based vaccine was able to partially or completely suppress HPV-related tumors.
Human papillomaviruses are the main cause of cervical cancer and also play a major role in head and neck tumors and other types of cancer. Preventive HPV vaccinations ward off infection with the pathogens and can thus prevent the development of cancer. However, there are currently no therapeutic vaccines that combat existing precancerous lesions or tumors.
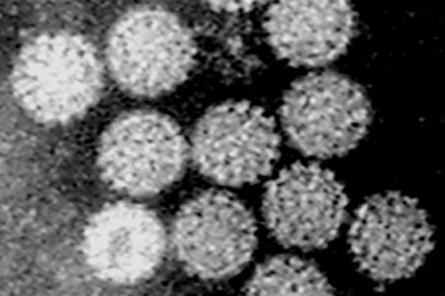
A new vaccination method developed by a research team led by Angelika Riemer from the DKFZ and the SILVACX* project group based at Heidelberg University relies on silica nanoparticles. This stable material, also known as silicon dioxide or silicic acid, has already proven itself in various medical applications. The silica particles are first coated to make them biocompatible. They are then loaded with short fragments of the viral proteins present in the cancer cells. To this end, the researchers select protein segments that are known to activate the human immune system.
After injection, specialized immune cells—known as antigen-presenting cells—take up the particles and present the viral epitopes on their surface. This activates cytotoxic T cells, which specifically recognize and destroy cancer cells. The combination with an additional adjuvant was particularly effective.
Humanized mice
The researchers used mice whose immune systems had been “humanized,” meaning they can present the same epitopes as humans. In these animals, the vaccination led to a significant activation of cytotoxic T cells. In some of the mice, existing HPV-positive tumors were completely suppressed, and these mice survived longer.
“These are encouraging results that confirm our decision to continue developing the nanoparticle vaccine system. It is versatile and could be used in the future not only against HPV-associated cancers, but also against other tumors or infectious diseases,” explains study leader Angelika Riemer.
Silica nanoparticles are the core element of the therapeutic vaccination process. They protect the vaccine epitopes in the body from rapid degradation, thus ensuring their bioavailability and uptake and presentation by immune cells. They are also characterized by their stability and ease of manufacture. Vaccines based on silica nanoparticles could therefore also be used in regions where it is difficult to maintain the refrigeration chain required for most vaccines – an important advantage for global application.
* SILVACX is funded by the EXIST program of the German Federal Ministry for Economic Affairs and Development.
Sebastian Kruse, Lia T. Fricke, Samantha Zottnick, Ann-Katrin Schlosser, Agnieszka K. Grabowska, Eva Feidt, Philipp Uhl, Ellen Junglas, Jonas D. Förster, Josephine Blersch, Philip Denner, Manina Günter, Stella E. Autenrieth, Eugenio Fava, Walter Mier, Armin Kübelbeck, and Angelika B. Riemer: A versatile silica nanoparticle platform for induction of T cell responses – applied for therapeutic vaccination against HPV16 E6/E7-positive tumors in MHC-humanized mice.
Oncoimmunology 2025, https://doi.org/10.1080/2162402X.2025.2548002






No comments yet