In 2022, the global landscape of HIV treatment remained challenging: approximately 9.2 million individuals with HIV were not undergoing treatment, and around 2.1 million were treated but did not achieve viral suppression.
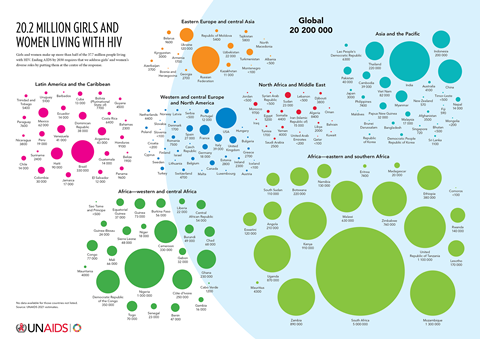
The situation is particularly dire in regions like Eastern Europe, Central Asia, the Middle East, and North Africa, where just about half of the over 2 million HIV-positive individuals had access to antiretroviral therapy. With nearly 25 million deaths and an estimated 33.2 million people (including 15.4 million women) living with the virus globally, HIV/AIDS is on the brink of becoming the most devastating pandemic the world has ever seen.
The global context of HIV/AIDS in women
The global impact of HIV/AIDS has been profound, with millions affected worldwide. However, its effect on women, particularly in specific regions, highlights a striking gender disparity. Notably, in sub-Saharan Africa, the prevalence of HIV among women is alarmingly high, a trend that’s been rising, emphasising the urgent need for prevention and treatment strategies tailored to women’s unique needs.
This disparity is further accentuated in regions like Eastern Europe and Central Asia, where socio-economic and cultural dynamics significantly increase women’s vulnerability to HIV. In these areas, societal norms and deep-rooted stigma not only fuel the spread of the virus among women but also hinder effective response and treatment efforts. The complexity of these factors necessitates a nuanced approach to HIV/AIDS that considers the specific challenges faced by women in different cultural and economic contexts. Such an approach must bridge the gap in healthcare access and education, ensuring that women in all regions have the tools and support necessary to combat this global health challenge.
Understanding the virology and biology of HIV in women
In understanding HIV transmission in women, it’s imperative to delve into the complex interplay of virological, biological, and immunological factors. The female reproductive tract (FRT) presents a unique landscape for HIV susceptibility due to its anatomical and physiological characteristics. The vaginal mucosa, owing to its extensive surface area and susceptibility to microabrasions during sexual intercourse, significantly increases the risk of HIV entry.
From a virological perspective, the transmission dynamics are influenced by the higher probability of viral transmission through the female genital tract compared to the male counterpart. This differential transmission rate can be attributed to a combination of anatomical susceptibility and the presence of specific immune cells that heighten vulnerability. For instance, certain subtypes of cervical Th17 CD4+ cells, characterised by the expression of HIV-enhancing factors such as CCR5, alpha4beta7, CD69, and IFN-gamma, amplify the risk of HIV infection in these regions.
Hormonal influences play a pivotal role in modulating the risk of HIV acquisition. Fluctuations in hormone levels, characteristic of menstrual cycles and pregnancy, can alter the immune landscape of the FRT. Hormones like oestrogen, known for their modulatory effects on the immune system, can influence HIV progression, potentially offering a protective effect under certain conditions. However, the relationship between hormonal fluctuations and HIV progression is complex, necessitating further exploration to unravel the underlying mechanisms.
Additionally, studies have indicated that women, on average, may present with higher baseline CD4 cell counts than men at the onset of antiretroviral therapy (ART). This difference, influenced by hormonal and immunological variances between sexes, suggests that women might experience a distinct trajectory of HIV progression. The nuanced interplay of sex hormones and innate immunity, affecting factors like epithelial permeability and cytokine secretion, further underscores the need for a gender-specific approach in HIV research.
Understanding the immune response in the FRT, especially considering the hormone-induced regulation of humoral, cell-mediated, and innate immune systems, is critical. It’s essential to recognise that immune cells in the FRT exhibit unique characteristics distinct from their counterparts in the systemic circulation. This distinction highlights the limitation of using systemic immune markers as surrogates for localised immune responses within the FRT.

Social and economic factors influencing women’s HIV risk
Gender discrimination and violence are significant factors that contribute to the vulnerability of women and girls to HIV. UNAIDS reports that AIDS remains the leading cause of death for women aged 15 to 49, with about 6,000 young women aged 15-24 contracting HIV every week. This alarming trend underscores the need for a global HIV response that prioritises gender equality and the empowerment of women and girls. The epidemic reflects the broader inequalities and injustices faced by women, where gaps in rights and services exacerbate their risk.
Women’s socio-economic status is directly linked to their HIV risk. Poverty and limited access to healthcare significantly impede their ability to access preventive measures or treatment. Intimate partner violence, prevalent in areas with high HIV prevalence, increases the risk of HIV infection in women by 50%. Additionally, being HIV-positive can lead to further violence, creating a vicious cycle that perpetuates the spread of HIV.
Education plays a crucial role in reducing HIV risk among women and girls. For example, in Botswana, extending mandatory secondary education was associated with a 12% reduction in girls’ risk of acquiring HIV. However, nearly one-third of the world’s poorest adolescent girls have never been in a classroom, highlighting the need for greater investment in women’s education as a means of HIV prevention.
The role of gender-based violence in HIV risk
Gender-based violence (GBV) is a pivotal factor in the spread of HIV among women, serving both as a cause and a consequence of the virus. It critically affects HIV clinical outcomes, including treatment adherence and retention, and is a substantial barrier to controlling the HIV epidemic. Statistically, one in three women worldwide experience physical or sexual violence in their lifetime, and women who experience intimate partner violence are 1.5 times more likely to acquire HIV.
In regions like Kenya and Uganda, intimate partner violence (IPV) has been linked to interruptions in PrEP adherence among HIV serodiscordant couples, with 23.8% of IPV survivors reporting PrEP interruptions compared to 6.9% of those not experiencing IPV. Similarly, a study in Zambia found that adolescents and young people who experienced high frequencies of violence had higher odds of viral load failure. In South Africa, only 25% of adolescents exposed to multiple types of violence adhered to HIV treatment in the past week, compared to 75% of their non-victimised peers.
The implications of GBV extend to HIV prevention and testing. Violence acts as a barrier to the initiation and adherence of PrEP. Additionally, women experiencing IPV may be less likely to access HIV testing services or disclose a positive HIV diagnosis due to fear of further violence. In terms of care and treatment, IPV can lead to lower CD4 counts, higher viral loads, and reduced treatment adherence in women and girls, further complicating their health outcomes.
Women’s participation in HIV research and clinical trials
Women, particularly Black women, are notably underrepresented in Phase III clinical trials for HIV treatments. This disparity is concerning given that women make up 19% of those newly diagnosed with HIV and nearly a quarter of people living with HIV in the United States. Such underrepresentation hampers our understanding of how HIV affects women differently and impedes the development of effective, gender-specific treatment and prevention strategies.
A review of women’s participation in Phase III trials submitted to the FDA since 2010 revealed that only 15% of participants were women. In the United States, this figure was even lower, with women comprising only 11% of trial participants. This lack of representation, particularly for Black women, means that clinical trials may not accurately reflect the efficacy and safety of HIV treatments for a significant portion of the HIV population. The overall participation-to-prevalence ratio (PPR) for U.S. women was 0.59, indicating a significant underrepresentation.
Research has shown that there are significant sex differences in treatment efficacy and safety outcomes, such as viral suppression and anaemia. However, the ability to detect these differences is limited by the low number of female participants. The reasons for women’s underrepresentation in trials are complex, including factors like lack of awareness, family responsibilities, and access barriers. Efforts to recruit and retain women in clinical trials have shown success when trials actively address these barriers.
Experts advocate for continued research into innovative methods to recruit and retain women in clinical trials. This includes involving key opinion leaders, investigators, and the HIV community in trial advisory boards and protocol review processes to ensure that trials are accessible and relevant to women.

Dr Ramya Kumar, an NIH Fogarty Global Health Fellow and Epidemiologist, shares her insights on the complex task of dismantling HIV-related stigmas in women, emphasizing the importance of both empathy and a deep understanding.
“HIV-related stigma is not just an issue of personal belief; it’s embedded within the fabric of families, communities, and healthcare systems,” she explains. “It’s a social process that involves labelling, stereotyping, and discrimination, often based on socially constructed notions of acceptability. To combat this, we need a comprehensive strategy that educates and cultivates empathy at multiple levels. HIV, a medical condition, should be approached with empathy, not judgment. Stigmatization, especially when it manifests as discrimination, can deter women from seeking testing and treatment.”
Strategies for effective HIV prevention and treatment in women
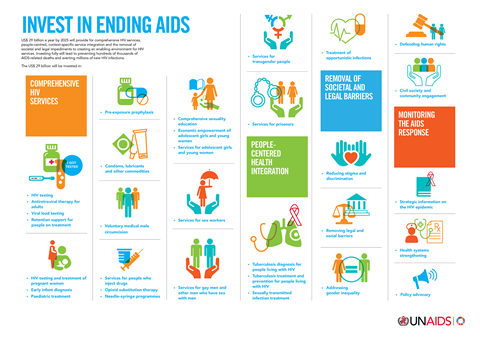
Prevention strategies for women must be uniquely designed to address their specific needs. This includes providing comprehensive sexual education and ensuring access to preventive tools such as condoms and PrEP (Pre-exposure prophylaxis). Addressing socio-economic barriers that hinder women’s access to these tools is also vital. The National Institutes of Health (NIH) emphasises the importance of including diverse populations of women in HIV prevention, treatment, and cure-related research as an essential step toward ending the HIV epidemic.
Ensuring access to quality healthcare is a critical aspect of HIV treatment for women. This means providing not only antiretroviral therapy but also comprehensive care that addresses the broader health needs of women, including reproductive health services. In 2023, the NIH Office of AIDS Research and the Office of Research on Women’s Health launched the HIV and Women Signature Program. This program focuses on an intersectional, equity-informed, data-driven approach to research on HIV in women, aiming to ensure that every woman receives care, prevention, and treatment tailored to her unique needs and circumstances.
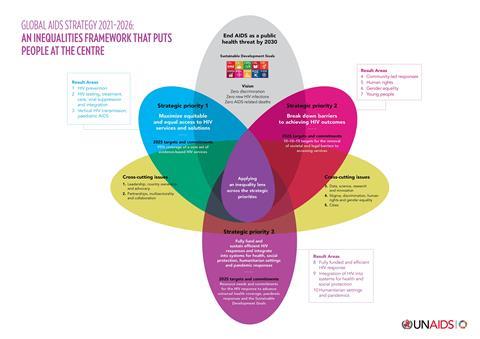
Policy and advocacy initiatives
Effective policy and advocacy initiatives are crucial in addressing the structural factors that increase women’s vulnerability to HIV. These initiatives should include policies that tackle gender inequality, support women’s economic empowerment, and promote gender-sensitive health services. The HIV and Women Signature Program, launched at the NIH OAR-ORWH Women & HIV Symposium, aims to identify gaps and priorities at the intersection of HIV and women’s health, indicating a proactive approach in shaping policies and advocacy efforts for women affected by HIV
A call to action
In conclusion, while significant strides have been made in understanding and treating HIV/AIDS, the unique challenges faced by women, particularly those of color and from resource-limited settings, remain a critical concern. This comprehensive analysis underscores the urgent need for tailored strategies that address the biological, socio-economic, and healthcare-specific needs of women.
We call upon healthcare policymakers, researchers, and advocates to prioritise gender-sensitive approaches in HIV/AIDS research and treatment. Efforts must focus on closing the gap in healthcare access, enhancing education and prevention strategies, and addressing the deeply entrenched socio-economic and cultural barriers that exacerbate women’s vulnerability to HIV/AIDS.
Together, through informed policymaking, dedicated research, and community-level advocacy, we can make significant progress toward reducing the impact of HIV/AIDS on women worldwide, ensuring a future where every woman has the opportunity to lead a healthy, empowered life, free from the burden of HIV/AIDS.
Further reading
Journal of the International AIDS Society publishes special issue on HIV and stigma - AIDS 2022
Sexuality and Reproduction in HIV-Positive Women: A Meta-Synthesis
Sex, gender and infectious disease | Nature Microbiology
A Systematic Review of the Inclusion (or Exclusion) of Women in HIV Research
Multimedia: Where Women Have No Doctor: A Health Guide for Women
Sex Differences in Immune Responses to Viral Infection | The Scientist Magazine® (the-scientist.com)
The Role of Gender in HIV Progression







No comments yet