The bacterium Acinetobacter baumannii is an extremely dangerous pathogen that is found, among other places, in hospitals: Many of the bacterial strains are resistant to different classes of antibiotics.
Infections with Acinetobacter baumannii were first observed on a greater scale during the Iraq War and have increased worldwide at a rapid pace ever since. This is the reason why the World Health Organization (WHO) has ranked Acinetobacter baumannii top of the list of bacteria for which new drugs are urgently needed.
However, the dangerous spread of Acinetobacter baumannii is not only due to antibiotic resistance but also to its enormous adaptability: It flourishes even under harsh conditions, such as desiccation and high salinity, and is therefore able to colonize different ecosystems in the human body such as the bladder, the surface of the skin and the lungs.
Research Unit (FOR) 2251 of the German Research Foundation, of which Professor Volker Müller of Goethe University Frankfurt is the spokesperson, has been studying the molecular basis of these adaptation strategies since 2017.
Adaptation mechanism
The research team led by Professor Beate Averhoff and Professor Volker Müller, the two FOR 2251 subproject leaders, has now discovered an adaptation mechanism previously unknown in Acinetobacter. When living conditions become inhospitable, many bacteria enter a dormant state that is almost death-like: They develop permanent forms with no metabolic activity. These are known as spores.
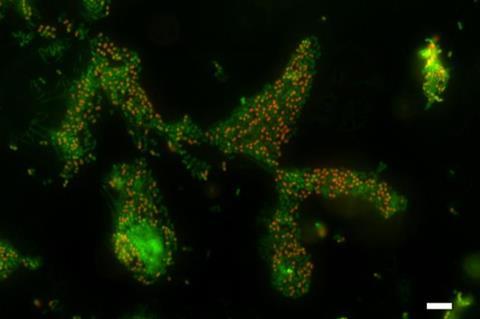
However, and as the research team discovered, Acinetobacter baumannii can form special cells as an alternative, which are in a kind of deep sleep. Although these cells still show signs of life and breathe, it is no longer possible to cultivate them on culture media in Petri dishes.
“We know this state from cholera bacteria, for example; it is referred to as the viable but non-culturable (VBNC) state,” explains Müller. Patricia König, the first author of the study, which was published recently in the renowned journal mBio, reports that the bacteria can survive for a long time in this state: “We have kept the bacteria in VBNC deep sleep for eleven months now and check regularly whether we can still wake them up. The study is still ongoing and there is no end in sight.”
Triggering deep sleep
The researchers were able to trigger the VBNC state in the Acinetobacter bacteria by raising the salt content of the culture medium, but also – with a time delay – through refrigerator (4 °C) and fever temperatures (42 °C), desiccation and by removing oxygen. In all cases, it was possible to “wake the bacteria up again” after two days of “rehab” in the shaker with an optimum supply of nutrients and oxygen.
The problem is that detecting bacteria by cultivating them on culture media is still the gold standard both in medicine as well as food control.
Beate Averhoff explains: “Imagine the following: A patient with an Acinetobacter baumannii infection is treated with antibiotics, and after seven days no more Acinetobacter bacteria grow on the Petri dishes. Doctor and patient assume that the bacterium has disappeared, but it is in fact just asleep in the nooks and crannies of the body, waiting to wake up again at the next, better opportunity, multiply and trigger symptoms in the patient again. This is extremely dangerous, particularly in the case of multidrug-resistant bacteria.”
More effective treatment
Patricia König says: “We hope that this will help us to contribute to developing more effective treatment concepts against Acinetobacter baumannii. Above all, we need to use more sensitive methods – in addition to Petri dishes – to detect it, such as PCR, which can also be used to spot VBNC cells.”
In terms of therapy, the proteins that appear to play an important role in the transition to the slumber state might constitute new entry points. The research team has already identified several such proteins.
König says: “We must learn to understand the role of these proteins. This will form the basis for developing inhibitors against them, which can be administered together with antibiotics to prevent the bacteria falling into a dangerous slumber.”







No comments yet