For a few dozen people in the world, the downside of living with a rare immune condition comes with a surprising superpower—the ability to fight off all viruses.
Columbia immunologist Dusan Bogunovic discovered the individuals’ antiviral powers about 15 years ago, soon after he identified the genetic mutation that causes the condition.
READ MORE: Study uncovers how Covid-19 is so good at defeating the innate immune response
READ MORE: Study maps main genes involved in immune response to infection by dengue virus
At first, the condition only seemed to increase vulnerability to some bacterial infections. But as more patients were identified, its unexpected antiviral benefits became apparent. Bogunovic, a professor of pediatric immunology at Columbia University’s Vagelos College of Physicians and Surgeons, soon learned that everyone with the mutation, which causes a deficiency in an immune regulator called ISG15, has mild, but persistent systemic inflammation.
“The type of inflammation they had was antiviral, and that’s when it dawned on me that these individuals could be hiding something,” Bogunovic recalls. When he and his colleagues looked at the individuals’ immune cells, they could see encounters with all sorts of viruses—flu, measles, mumps, chickenpox. But the patients had never reported any overt signs of infection or illness.
Light immune activation
“In the back of my mind, I kept thinking that if we could produce this type of light immune activation in other people, we could protect them from just about any virus,” Bogunovic says.
Today, Bogunovic is closing in on a therapeutic strategy that could provide that broad-spectrum protection against viruses and become an important weapon in next pandemic.
In his latest study, published Aug. 13 in Science Translational Medicine, Bogunovic and his team report that an experimental therapy they’ve developed temporarily gives recipients (hamsters and mice, so far) the same antiviral superpower as people with ISG15 deficiency. When administered prophylactically into the animals’ lungs via a nasal drip, the therapy prevented viral replication of influenza and SARS-CoV-2 viruses and lessened disease severity.
In cell culture, “we have yet to find a virus that can break through the therapy’s defenses,” Bogunovic says.
Immune superpowers
Bogunovic’s therapy is designed to mimic what happens in people with ISG15 deficiency, but only for a short time.
Instead of turning off ISG15 directly—which leads to the production of more than 60 proteins—Bogunovic’s therapeutic turns on production of 10 proteins that are primarily responsible for the broad antiviral protection.
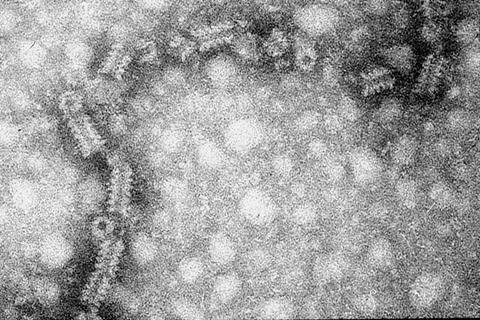
The current design resembles COVID mRNA vaccines but with a twist: Ten mRNAs encoding the 10 proteins are packaged inside a lipid nanoparticle. Once the nanoparticles are absorbed by the recipient’s cells, the cells generate the ten host proteins to produce the antiviral protection.
“We only generate a small amount of these ten proteins, for a very short time, and that leads to much less inflammation than what we see in ISG15-deficient individuals,” Bogunovic says. “But that inflammation is enough to prevent antiviral diseases.”
Foundation for future therapy
Bogunovic’s team sees their technology as a weapon for the next pandemic—providing protection for first responders, people in nursing homes, and family members of infected individuals—regardless of the responsible virus.
“We believe the technology will work even if we don’t know the identity of the virus,” Bogunovic says. Importantly, the antiviral protection provided by the technology will not prevent people from developing their own immunological memory to the virus for longer-term protection.
But the technology’s drug delivery and absorption properties still need optimization. When delivered to animals via nanoparticles, the 10 proteins were produced in the lungs, “but probably not at high enough levels that makes us comfortable going into people immediately,” Bogunovic says.
Delivering the therapy
“Once the therapy reaches our cells, it works, but the delivery of any nucleic acid, DNA or RNA, into the part of the body you want to protect is currently the biggest challenge in the field.” The researchers also need to determine how long the therapy’s antiviral protection will last, currently estimated at three to four days.
“Our findings reinforce the power of research driven by curiosity without preconceived notions,” Bogunovic says. “We were not looking for an antiviral when we began studying our rare patients, but the studies have inspired the potential development of a universal antiviral for everyone.”
The study, “An mRNA-based broad-spectrum antiviral inspired by ISG15 deficiency protects against viral infections in vitro and in vivo,” was published Aug. 13 in Science Translational Medicine.
Dusan Bogunovic reports ownership in Lab11 Therapeutics.






No comments yet