Tuberculosis, often thought of as a disease of the past, is making a resurgence across the United States. Arizona State University researchers have made a discovery that could help stop it.
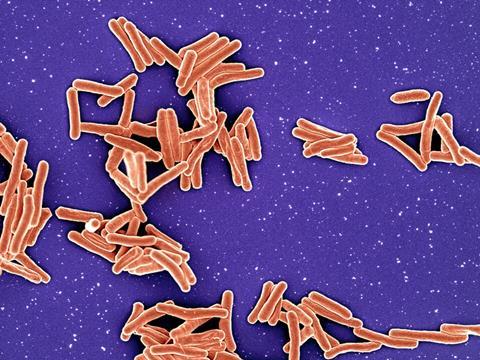
Scientists from ASU’s School of Life Sciences and the Biodesign Institute’s Center for Bioelectronics and Biosensors have identified a molecular system inside Mycobacterium tuberculosis that functions like the organism’s heart or lungs, keeping it alive.
The system, known as PrrAB, helps the bacterium generate energy and breathe. When researchers used a gene-silencing tool called CRISPR interference, or CRISPRi, to turn off PrrAB, the bacteria died.
“It’s absolutely critical and essential for the life of the organism,” said Shelley Haydel, a professor in ASU’s School of Life Sciences and senior author of the study. “If your heart stopped working right now, you’d die. That’s what this system is for the TB bacterium.”
READ MORE: New study finds targets for a new tuberculosis vaccine
READ MORE: Breathing new life Into TB treatment with inhalable nanomedicine
The findings, published in ACS Infectious Diseases, could help pave the way for new tuberculosis treatments.
Power source
In tuberculosis bacteria, PrrAB regulates genes that control respiration and energy production. Without it, the cells cannot survive. Postdoctoral researcher Yannik Haller, the study’s first author, compared the system to the power cord of a CD player.
“If you look at a CD player, the CD is the main medium,” Haller said. “But you need power. PrrAB is kind of like the power cord that powers the CD player. If you take that power away, nothing works.”
Because humans do not have this kind of system, drugs that target PrrAB could potentially kill the bacterium without harming human cells.
DAT-48: a compound that kills tuberculosis
The ASU team also studied an experimental compound called diarylthiazole-48, or DAT-48, that acts through the PrrAB system. In laboratory tests, DAT-48 killed several strains of M. tuberculosis, including clinical ones. It did not affect related species such as Mycobacterium abscessus, suggesting the compound is selective for TB.
“DAT-48 is really exciting because we’ve tried it in multiple different drug combinations,” Haller said. “They actually work better together than by themselves, and there’s what we call synergy.”
The researchers found that combining DAT-48 with existing TB drugs such as bedaquiline and telacebec produced stronger results than using any of the drugs alone. This combination strategy could make treatment faster and more effective.
Haydel said the results reinforce the idea that PrrAB is a promising target for new tuberculosis drugs. “For many years, we would say, ‘This is essential for TB to live; it’s a great drug target,’” she said. “And now, there’s evidence that it really is.”
Rising threat
After years of decline, tuberculosis cases have begun to rise again in parts of the United States.
“The most recent cases in Kansas City are the largest outbreak ever recorded in the U.S.,” Haller said. “There’s about 120 confirmed cases and more than 100 people undergoing therapy. For this outbreak, there’s no direct link to travel.”
Haller added that many people underestimate how widespread TB remains. “About one in four people around the globe have been infected with TB,” he said. “It’s a huge global problem. People don’t realize how big of an issue it actually is.”
Haydel noted that while the Kansas City outbreak was not drug-resistant, multidrug-resistant TB has appeared elsewhere in the world and could become a problem in the U.S. “Being ready and having an arsenal of new drugs for TB is important,” she said. “This research could help us prepare.”
Next steps in the lab
The ASU team plans to continue studying DAT-48 and the PrrAB system. Haller said the researchers hope to use artificial intelligence to improve the molecule and design better versions more quickly. “With computation, we can predict how a compound might behave in humans and make improvements before we even test it,” he said. “The field is moving toward AI-assisted design because it allows really high-throughput screening in a short time.”
Haydel said the team is eager to advance the work but needs financial support. “We’ve been working on this project for seven years without any direct federal funding,” she said. “We’ve pieced it together. Now we need funding support to move it forward.”
For Haydel, who has studied tuberculosis for more than three decades, the project represents a milestone. “I started working on TB right out of college,” she said. “It’s one of the infectious diseases that I love studying because it’s complex and it matters.”
Haller added that the ultimate goal is simple: to make sure tuberculosis does not regain a foothold. “TB anywhere is a problem everywhere,” he said. “We’re trying to make sure we have the tools ready before it becomes one again.”






No comments yet