An agricultural fungicide approved in the US and currently under consideration by authorities worldwide could have a devastating effect on a new drug for one of world’s deadliest infectious diseases, show University of Manchester scientists.
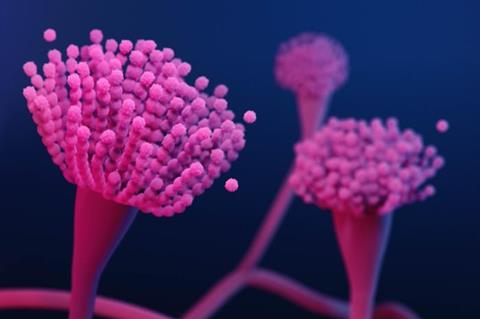
Their Wellcome Trust funded study, published in Nature Microbiology could spell disaster for patients with aspergillosis - a dangerous fungal disease responsible for the deaths of millions of people worldwide.
With few treatment options for patients, aspergillus has developed widespread drug resistance to one class of drugs, known as the azoles.
The resistance is caused by the use of fungicides in agriculture, known as DMIs, increasing the risk of mortality from aspergillosis from 40% to up to 80%.
Antifungal drug
However, F2G Ltd – a spin out company from The University of Manchester – invested more than £250 million over 20 years on a new antifungal drug called olorofim, which is in late-stage clinical trials and aims to be clinically deployed within the next few years.
The scientists argue that because olorofim works against azole resistant infections it could save many lives of affected patients.
However, a newly developed fungicide crop spray called ipflufenoquin has been approved for use in the USA, under the trade name Kinoprol, and could severely impact on the new drug because it has the same biological target and kills the fungi the same way as olorofim.
Threat to drug
Exposure of Aspergillus in the environment to Kinoprol could make it resistant to olorofim, rendering the treatment ineffective before it can even be deployed in the clinic, say the scientists.
The research team exposed Aspergillus to ipflufenoquin in the lab and then assessed resistance to olorofim. Genetic mutations that cause changes in the antifungals target gene provide resistance to ipflufenoquin but also provide resistance to olorofim.
Scientists have long known that environmental use of fungicides – which farmers need to keep their crops free of fungal infection – has the potential to drive resistance to other clinical antifungals.
Researchers also believe that composting of waste from farms is causing accumulation of fungicides in environments where Aspergillus likes to grow.
Dispersal of spores
Wind currents, intensive farming, and transport of commercial composts can disperse the drug-resistant fungal spores further into the environment and end up in our gardens, bedrooms, kitchens, and bathrooms.
Most healthy people are unaffected by Aspergillus, but population groups including the elderly, cancer patients, and the immunosuppressed of all ages are at greater risk of serious illness which destroys the lungs.
Lead author Dr Norman van Rhijn, a Wellcome Trust research fellow at The University of Manchester said: “We are all very excited about olorofim but when we found out that regulatory approval was sought for ipflufenoquin and its mode of action was same as olorofim, we immediately felt alarmed.
Desperately needed
“Making a novel fungicide for humans is very difficult and costs millions of pounds.
“But it is desperately needed, as the few classes of drugs for Aspergillus infection available at present don’t give all of the seriously ill patients a viable treatment option.
“That is why olorofim is such an exciting prospect for patients and why we must lobby the regulatory authorities to implement a risk assessment strategy for the dual use of antifungals in agriculture and clinic.”
“But indirect implications to human health are not taken into account during the approval process, which is why researchers, collaborators, and clinical teams are lobbying hard for the authorities to risk assess any new fungicide.
Lack of legislation
Corresponding author Prof Mike Bromley, who is a former employee of F2G Limited and co-lead of the Fungal AMR and One Health Network, said: “It is devastating that the efforts that so many have made in development of olorofim are being put at risk by the lack of appropriate legislation that would prevent the release of fungicides without consideration of the risks to driving drug resistance in human pathogens.
“We have made our views clear to the Environmental Protection Agency in the USA and hope they will re-evaluate their approach to environmental release of fungicides.
Political debate
Politicians in the House of Lords recently debated a question by Baroness Bennett of Manor Castle, which asked the Government what assessment they made of how the UK’s current agricultural fungicide use will affect long-term food and biological security.
Baroness Bennett, a former leader of the Green Party, told the chamber: “Managing fungal crop disease has always been essential to our ability to feed the population, but we cannot afford a haphazard, piecemeal approach that will hurt our public health and our NHS.
“We need integrated, “one health” considerations of the impact of the climate emergency and responsible fungicide legislation.”
Baroness Hayman of Ullock and Baroness Walmsley also spoke in the debate, and highlighted the specific case of olorofim and ipflufenoquin as they called for more robust risk assessments in the licensing of new agricultural antifungals.
F2G carried out a single assay in the study that the researchers would otherwise have not been able to facilitate. However, the vast majority of the study was carried out independently.
Topics
- Agriculture
- Antimicrobial Resistance
- Antimicrobials
- aspergillosis
- Aspergillus
- azoles
- F2G Ltd
- Fungi
- House of Lords
- Infection Prevention & Control
- ipflufenoquin
- Kinoprol
- Medical Microbiology
- Mike Bromley
- Norman van Rhijn
- olorofim
- One Health
- Research News
- Soil & Plant Science
- UK & Rest of Europe
- University of Manchester
- USA & Canada







No comments yet