Researchers at the Icahn School of Medicine at Mount Sinai and collaborators have reported early success with a novel mRNA-based therapy designed to combat antibiotic-resistant bacteria.
The findings, published in the November 26 online issue of Nature Biotechnology, show that in preclinical studies in mice and human lung tissue in the lab, the therapy slowed bacterial growth, strengthened immune cell activity, and reduced lung tissue damage in models of multidrug-resistant pneumonia.
Antibiotic-resistant infections are a growing global threat, killing more than 1.2 million people each year and contributing to nearly 5 million deaths worldwide. In the United States alone, more than 3 million infections occur annually, causing up to 48,000 deaths and costing billions of dollars in health care. Experts warn that resistance is increasing across nearly all major bacterial species, putting routine surgeries, cancer treatments, and newborn care at risk.
READ MORE: Safer, more effective vaccines with new mRNA vaccine technology
READ MORE: Groundbreaking study shows potential of new mRNA vaccine to help fight tuberculosis
“Our work suggests there may be a new path to tackling antibiotic-resistant infections by supporting the immune system more directly,” says Xucheng Hou, PhD, a lead author of the study and Assistant Professor of Immunology and Immunotherapy in the lab of Yizhou Dong, PhD, at the Icahn School of Medicine at Mount Sinai. “Although we’re still in the early stages and have only tested this approach in preclinical models, the results lay important groundwork for future therapies that could enhance how traditional antibiotics perform.”
Break down and recruit
The experimental therapy works by giving the patient mRNA that instructs their body to make a special infection-fighting protein called a “peptibody.” This peptibody is designed to do two things at the infection site: directly break down harmful bacteria and recruit immune cells to help clear them out.
To get the mRNA safely into the patient’s body, the researchers packaged it inside lipid nanoparticles—tiny fat-based bubbles commonly used in mRNA vaccines. These nanoparticles protect the mRNA as it travels through the body and help it enter cells. They also carry an extra ingredient that helps limit harmful inflammation by neutralizing excess reactive oxygen species, highly reactive molecules that the body produces during infection and that can damage tissues, often contributing to the severe symptoms of hard-to-treat infections.
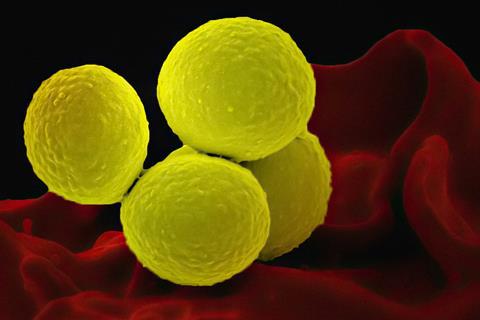
In mouse models of multidrug-resistant Staphylococcus aureus and Pseudomonas aeruginosa, repeated doses of the therapy were well tolerated, reduced bacterial numbers in the lungs, decreased inflammation, and preserved normal lung structure, the investigators report. In addition, the laboratory tests with human lung tissue showed similar results, demonstrating that the therapy could work alongside human immune cells.
Next steps
Next, the researchers plan to continue preclinical studies and eventually advance toward human clinical trials to evaluate safety, dosing, and efficacy. While the therapy is still in early stages, it represents an encouraging direction in the global fight against antibiotic-resistant infections.
“This is the first evidence that an mRNA-encoded antimicrobial peptide can directly kill bacteria while also turning on the immune system’s protective responses,” says Dr. Dong, the senior author and a co-corresponding author of the study, Mount Sinai Professor in Nanomedicine, and a member of the Icahn Genomics Institute and the Marc and Jennifer Lipzhultz Precision Immunology Institute (PrIISM) at the Icahn School of Medicine at Mount Sinai. “If future studies bear this out, it could open the door to a highly adaptable platform for developing new treatments against infections that no longer respond to today’s antibiotics.”
The paper is titled “Antimicrobial peptide delivery to lung as peptibody mRNA in anti-inflammatory lipids treats multidrug-resistant bacterial pneumonia.”
The study’s authors, as listed in the journal, are Yonger Xue, Xucheng Hou, Siyu Wang, Yuebao Zhang, Yichen Zhong, Diana D. Kang, Chang Wang, Haoyuan Li, Changyue Yu, Zhengwei Liu, Meng Tian, Dinglingge Cao, Ya Ying Zheng, Binbin Deng, Pauline Hamon, Miriam Merad, and Yizhou Dong.
This work is supported, in part, by the Maximizing Investigators’ Research Award (R35GM144117) from the National Institute of General Medical Sciences.
Topics
- Antimicrobial Resistance
- Bacteria
- Clinical & Diagnostics
- Icahn School of Medicine at Mount Sinai
- Immunology
- Infection Prevention & Control
- Infectious Disease
- Medical Microbiology
- mRNA therapies
- One Health
- peptibodies
- Pharmaceutical Microbiology
- Pseudomonas aeruginosa
- Research News
- Staphylococcus aureus
- USA & Canada
- Xucheng Hou
- Yizhou Dong







No comments yet