In a modeling study of women vaccinated against human papillomavirus (HPV), researchers found that cervical cancer screening could be done far less often than current recommendations without compromising health benefits.
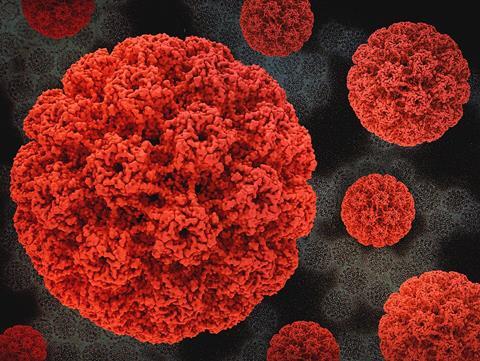
For women vaccinated at younger ages, screening just two or three times over a lifetime was both cost‑effective and associated with fewer unnecessary follow‑up procedures, suggesting that existing screening guidelines may be overly intensive for this growing population. The study is published in Annals of Internal Medicine.
Researchers from the University of Oslo, Harvard T.H. Chan School of Public Health, and the National Cancer Institute used individual‑based computer modeling and published data to evaluate different cervical cancer screening strategies for women in Norway who received HPV vaccines between the ages of 12 and 30.
The model-based analysis compared varying ages to start screening, screening intervals, and total lifetime tests, while accounting for health care costs and patient time. Across all vaccination ages and vaccine types, less frequent screening was consistently preferred.
Less intensive screening
For women who received the vaccine by age 30, a far less intensive screening program would be more cost-effective and cause less harm than the current recommendation of screening every five years. For women vaccinated before age 25, preferred strategies involved screening every 15 to 25 years, resulting in screening 2 to 3 times over a lifetime.
READ MORE: New research confirms HPV vaccination prevents cervical cancer
READ MORE: Hidden HPV-linked cell type may drive early cervical cancer, scientists report
These findings held true even when researchers accounted for missed screenings or reduced vaccine protection. The study concludes that cervical cancer screening programs could be tailored based on a woman’s age at HPV vaccination, improving value while reducing harm.







No comments yet