A new study in Nature shows that delivering a single injection of gene therapy at birth may offer years-long protection against HIV, tapping into a critical window in early life that could reshape the fight against pediatric infections in high-risk regions.
This study is among the first to show that the first weeks of life, when the immune system is naturally more tolerant, may be the optimal window for delivering gene therapies that would otherwise be rejected at older ages.
READ MORE: Report: Critical gaps continue to undermine efforts to end AIDS in children
READ MORE: Very early antiretroviral therapy within hours of birth could suppress HIV in newborns
“Nearly 300 children are infected with HIV each day,” said first author Amir Ardeshir, associate professor of microbiology and immunology at the Tulane National Primate Research Center, who conducted the study alongside fellow researchers at the California National Primate Research Center. “This approach could help protect newborns in high-risk areas during the most vulnerable period of their lives.”
Gene therapy
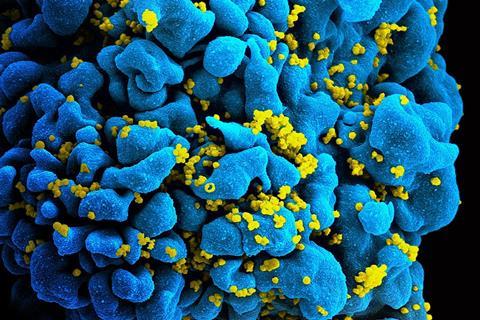
In the study, nonhuman primates received a gene therapy that programs cells to continuously produce HIV-fighting antibodies. Timing proved critical to the one-time treatment offering long-term protection.
Those that received the treatment within their first month of life were protected from infection for at least three years with no need for a booster, potentially signifying coverage into adolescence in humans. In contrast, those treated at 8-12 weeks showed a more developed, less tolerant immune system that did not accept the treatment as effectively.
“This is a one-and-done treatment that fits the critical time when these mothers with HIV in resource-limited areas are most likely to see a doctor,” Ardeshir said. “As long as the treatment is delivered close to birth, the baby’s immune system will accept it and believe it’s part of itself.”
Mother-to-child transmission
More than 100,000 children acquire HIV annually, primarily through mother-to-child transmission after birth from breastfeeding. Antiretroviral treatments have shown success in suppressing the virus and limiting transmission, however adherence to treatment and access to doctors both decline after childbirth, particularly in areas with limited access to healthcare.
To deliver the treatment, researchers used an adeno-associated virus (AAV), a harmless virus that can act as a cargo truck to deliver genetic code to cells. The virus was sent to muscle cells, unique in their longevity, and delivered instructions to produce broadly neutralizing antibodies, or bNAbs, which are capable of neutralizing multiple strains of HIV.
This approach solved a longstanding problem with bNAbs. Previous studies found them effective at fighting HIV, but they required repeated infusions, which are costly and pose logistical challenges in low-resource settings.
Micro factories
“Instead, we turn these muscle cells — which are long-lived — into micro factories that just keep producing these antibodies,” Ardeshir said.
Newborns showed greater tolerance and expressed high levels of bNAbs, which successfully prevented infection during simulated breastfeeding and later exposures mimicking sexual transmission. Older infants and juveniles were more likely to have produced anti-drug antibodies that shut down the treatment.
Researchers also found that exposing fetuses to the antibodies before birth helped older infants accept the gene therapy later, avoiding the immune rejection that often occurs with age.
One-time injection
Still, Ardeshir said a one-time injection at birth offered a more cost-effective and feasible real-world solution, while putting less burden on the mother for a follow-up visit.
Questions remain as to how the results translate to human infants and children, who may be less susceptible to AAV-delivered treatments. The study also used one strain of simian–human immunodeficiency virus, which doesn’t reflect the variety of HIV strains.
If successful, however, this treatment could dramatically reduce mother-to-child HIV transmission rates in high-risk regions such as sub-Saharan Africa, where 90% of pediatric HIV cases can be found. It may also be adapted to protect against other infectious diseases like malaria, which disproportionately affects young children in low-income countries.
Huge result
“Nothing like this was possible to achieve even 10 years ago,” Ardeshir said. “This was a huge result, and now we have all the ingredients to take on HIV.”
This research was supported with resources from the Tulane National Primate Research Center base grant of the National Institutes of Health, P51OD011104 and the base grant of the California National Primate Research Center, P51OD011107.
Topics
- adeno-associated virus
- Amir Ardeshir
- antibodies
- broadly neutralizing antibodies
- California National Primate Research Center
- Disease Treatment & Prevention
- Economic Equality
- gene therapy
- HIV
- Immunology
- Infection Prevention & Control
- Infectious Disease
- newborns
- One Health
- Research News
- Tulane National Primate Research Center
- USA & Canada
- Viruses







No comments yet