Recovery from deadly influenza infection may hinge on helping the lungs heal in addition to stopping the virus, according to a new study in mice, which shows that pairing modest antiviral therapies with immune modulation can restore damaged tissues and lung function, even after severe infection has taken hold.

The findings, published in Science, offer a foundation for future clinical strategies to improve outcomes in severe acute respiratory disease once standard treatments are no longer sufficient. Despite the availability of vaccines and antiviral drugs, severe lung infections, like influenza and COVID-19, can lead to severe disease, including pneumonia and acute respiratory distress syndrome.
Severe and fatal cases of these maladies are often driven not only by the virus itself, but by a harmful inflammatory cascade that can lead to tissue damage and loss of lung function. Most current treatments for these diseases target inflammation or viral replication alone and tend to fail once extensive tissue damage has already occurred. As a result, therapies for late-stage disease are currently lacking.
The timing of disease
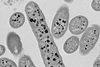
To better understand the timing of disease process and the balance between tissue injury and repair in severe pulmonary infection, Hiroshi Ichise and colleagues evaluated more than 50 immunomodulatory approaches in a lethal mouse influenza model and found that none improved survival when applied alone, except for neutrophil depletion.
Given these observations, Ichise et al. propose a “tipping point” model – once early viral and inflammatory damage passes a certain threshold, controlling inflammation alone cannot restore tissue function. They argue that late in the course of viral pneumonia, and perhaps other acute respiratory diseases, recovery depends on rebalancing tissue injury and repair, rather than suppressing inflammation or viral replication.
To test recovery-focused strategies, Ichese et al. combined partial viral control and either a blockade of interferon signaling to enhance repair or depletion of cytotoxic T Cells (CD8+) to limit immune-mediated damage. Through both molecular and imaging analyses, the authors show that both regimens successfully reduced lethality by preserving or restoring tissue integrity and lung function.






No comments yet