A new review, led by first author Hashim Muhammad Moseeb and corresponding author Zahoor Kamran from the University of Missouri-Columbia, explores how changes in the gut microbiome are associated with the development of obesity, metabolic syndrome, and colorectal cancer in the United States (U.S.) population.

It highlights growing scientific evidence that imbalances in gut bacteria can influence metabolism, trigger inflammation, and increase cancer risk. These insights offer new possibilities for disease prevention, early detection, and personalized health care.
The review was published in Volume 12 of Oncoscience on November 7, 2025, titled “From obesity to cancer: Gut microbiome mechanisms, biomarkers, and U.S. public health strategies.”
Obesity and colorectal cancer remain major public health concerns in the U.S. Over 40% of U.S. adults are classified as obese, and colorectal cancer is one of the leading causes of cancer-related deaths. This review emphasizes that the trillions of microbes living in the human digestive tract, known as the gut microbiome, may play a key role in developing these health outcomes. Disruptions in this microbial balance, often driven by Western diets, environmental exposures, and lifestyle habits, may promote inflammation and harmful metabolic changes.
Early disease signals
The review highlights specific bacteria, such as Fusobacterium nucleatum and Escherichia coli, that are associated with colorectal cancer through mechanisms like DNA damage, chronic inflammation, and immune suppression. In obesity, the presence of pro-inflammatory bacteria and reduced microbial diversity are associated with insulin resistance and fat buildup. These findings are supported by major U.S. cohort studies, including the Nurses’ Health Study and NHANES, which now incorporate microbiome data to track early disease signals.
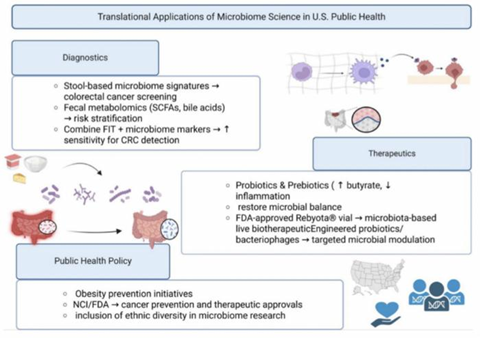
The authors also explore promising strategies for public health and clinical care. These include stool-based microbiome screening tests for colorectal cancer, dietary changes to improve gut health, and new microbiota-based treatments. The recent FDA approval of therapies like Rebyota® reflects growing interest in microbiome-based medicine. Diet remains a powerful tool, as fiber-rich foods support beneficial bacteria and may help reduce cancer risk.
Diverse representation
Importantly, the review discusses how microbiome-related diseases affect different racial and socioeconomic groups. Diverse representation in microbiome research is essential to ensure health equity and effective care for all populations. The authors advocate for better integration of microbiome science into national policies on diet, cancer screening, and chronic disease prevention.
READ MORE: Circadian rhythms as a modulator of gut microbiota-tumor microenvironment crosstalk
READ MORE: Engineered gut bacteria improves survival outcomes in colorectal cancer tumors
“The emerging discipline of Molecular Pathological Epidemiology (MPE) integrates lifestyle, microbiome, and biomarker data to elucidate exposure-outcome relationships, enabling personalized prevention and therapeutic strategies.”
By connecting gut health to two of the most serious chronic diseases in the U.S., this review provides a valuable guide for how microbiome research can support public health. It also highlights the need for continued research, population-based studies, and inclusive prevention strategies that benefit all communities.
Topics
- Bacteria
- biomarkers
- Cancer Microbiology
- Cardiometabolic disease
- colorectal cancer
- Disease Treatment & Prevention
- Escherichia coli
- Fusobacterium nucleatum
- Gut Microbiome
- Hashim Muhammad Moseeb
- Immunology
- inflammation
- metabolic syndrome
- Molecular Pathological Epidemiology
- obesity
- One Health
- Rebyota
- Research News
- University of Missouri-Columbia
- USA & Canada
- Zahoor Kamran







No comments yet